Oral Cancer
What are the Risk Factors of Oral Cancer?
How to prevent oral cancers?
How does oral cancer present?
How to diagnose Oral Cancer?
How is a biopsy done?
What are the other tests to be done if the biopsy is positive?
Where does oral cancer spread?
How common is oral cancer?
What is the probability that the patient with oral cancer is cured?
What are the treatment modalities to treat Oral Cancers?
How is surgery for oral cancer done, and how does it help?
Wide local excision
Lymph Node Dissection
Reconstruction of the tumours
What is the need for reconstruction after removal of oral cancer?
How do we reconstruct after surgical removal of tumour?
What are the complications of surgery?
What is expected in the post-operative period?
What are the long term problems with oral cancer?
When will radiotherapy be necessary?
When will chemotherapy be necessary?
When will Targeted therapy be used?
Can Oral Cancer come back? How can one identify the same?
How will recurrence be treated?
What is cancer?
- Cells are the basic building blocks of the tissues and organs of our body. Usually, these cells divide to make new cells in a controlled manner, and beyond a point, the cells are replaced with new cells. This is how our bodies grow, heal and repair. Sometimes, this orderly growth of cells can go wrong due to the mutation or sudden change in the genes which control how cells behave. This can make the cells divide abnormally, producing more abnormal cells, forming a lump called a tumour. These cells cannot stay together, can easily detach from each other and spread via direct contact, lymphatics and bloodstream to different organs in the body.
What are the Risk Factors of Oral Cancer?
- Tobacco (Smoking and Oral forms such as Gutka, Panmasala, Betel Nut)
- Alcohol
- Sharp tooth
- Ill-fitting Dentures
- Spicy food
- Human Papilloma Virus (HPV) infection
- Sunlight (Ultraviolet Radiation)
- Weak immune system (HIV, transplant recipients)
How to prevent oral cancers?
- Limit smoking and Alcohol
- HPV vaccines
- Healthy diet
- Maintaining good oral hygiene
- Properly fitted dentures
- Grinding of the sharp tooth and prevent recurrent trauma
- Oral screening of high-risk population and treatment of premalignant lesions.
How does oral cancer present?
- Oral Cancers most commonly presents as an ulcer or as a proliferative lesion in the oral cavity that does not heal within two weeks. Oral cancers increase in size and bleed on touch. Any ulcer or a proliferative lesion in the mouth that does not heal within two weeks has to be examined by the doctor and must rule out malignancy. They may occasionally present with difficulty in opening the mouth, speaking, swallowing, loosening of teeth, swellings in the neck, ear pain and bad breath.
How to diagnose Oral Cancer?
- Oral cancers can be easily identified with a good history and clinical examination. Suspicious lesions need to be confirmed by taking a biopsy. A small piece of tissue is taken from the lesion and sent to the lab to confirm the diagnosis.
How is a biopsy done?
- The biopsy is usually done under local anaesthesia. Local anaesthesia is either sprayed over the biopsy site or injected around the ulcer to make the area numb. Once there is no pain at the biopsy site, a small portion of the lesion is removed and sent to the lab to be seen under the microscope. There may be a bit of bleeding that will usually settle down on pressure. Sutures are rarely required. The results of the biopsy will come within 2 to 3 days.
What are the other tests to be done if the biopsy is positive?
- CT Scan/MRI Scan of the head and neck, and chest To know the extent of the tumour, a CT scan or MRI scan of the head and neck and chest may be taken
- FNAC ( Fine Needle Aspiration Cytology) of the lymph nodes To know whether the swellings in the neck (Lymph Nodes) are involved due to the tumour, FNAC ( Fine Needle Aspiration Cytology) of the lymph nodes can be done.
- Endoscopy At times, endoscopy may be done to know whether any other part of the oropharyngeal tract is involved.
Where does oral cancer spread?
- Oral cancer initially spreads to the lymph nodes in the neck. Then, it can further spread to the lungs and the bone.
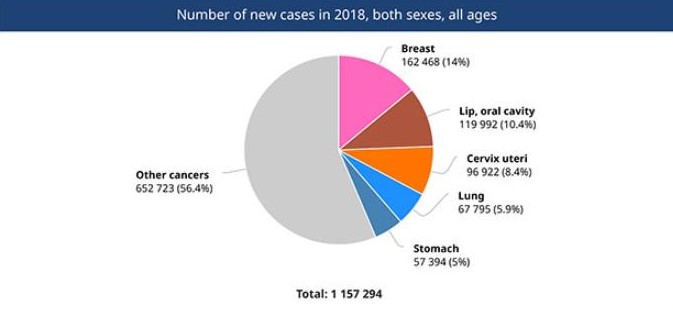
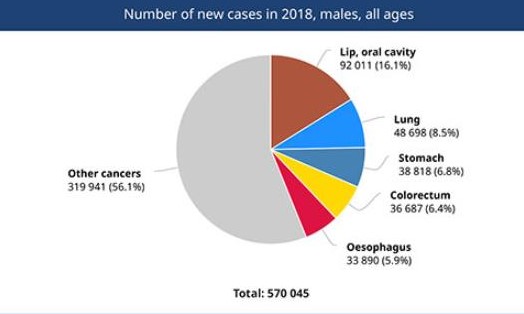
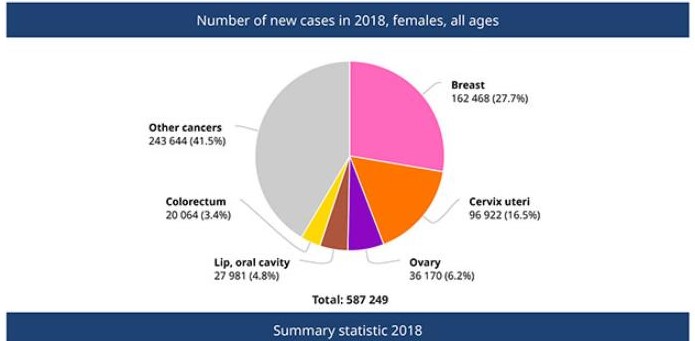
How common is oral cancer?
- Oral cancer is very common. Oral cancers are the second leading cause of cancer in India after breast cancer. Around one-third of oral cancer cases in the world is present in India. Oral cancer is the most common cancer in men. It accounts for 16% of all cancers in men and 10% of all cancers in both men and women in India.
What is the probability that the patient with oral cancer is cured?
- The possibility of survival depends on the cancer stage, site of involvement, grade of the tumour and the patient’s compliance with the treatment. The survival of patients with cancer is generally denoted as 5-year survival, wherein the percentage of people surviving at the end of 5years after a cancer diagnosis is noted down. This is given in the tabular column below.
5-year survival rate.
| Lip | Tongue | Buccal Mucosa | Floor Of Mouth | |
|---|---|---|---|---|
| Stage I and II: | >92% | 81% | 85% | 77% |
| Stage III: | >60% | 68% | 62% | 38% |
| Stage IV: | 28% | 39% | 50% | 20% |
What are the treatment modalities to treat Oral Cancers?
- Various treatment modalities like surgery, chemotherapy, radiotherapy, and targeted therapy help treat oral cancer. When the patient presents early ( Stage 1 and 2), the patients can be treated by either surgery or radiotherapy depending on the tumour site. In advanced stages ( Stage 3&4), the patients might be treated with a combination of surgery, radiotherapy and chemotherapy to attain the best results.
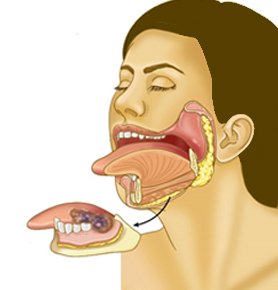
How is surgery for oral cancer done, and how does it help?
- Surgery for oral cancer involves
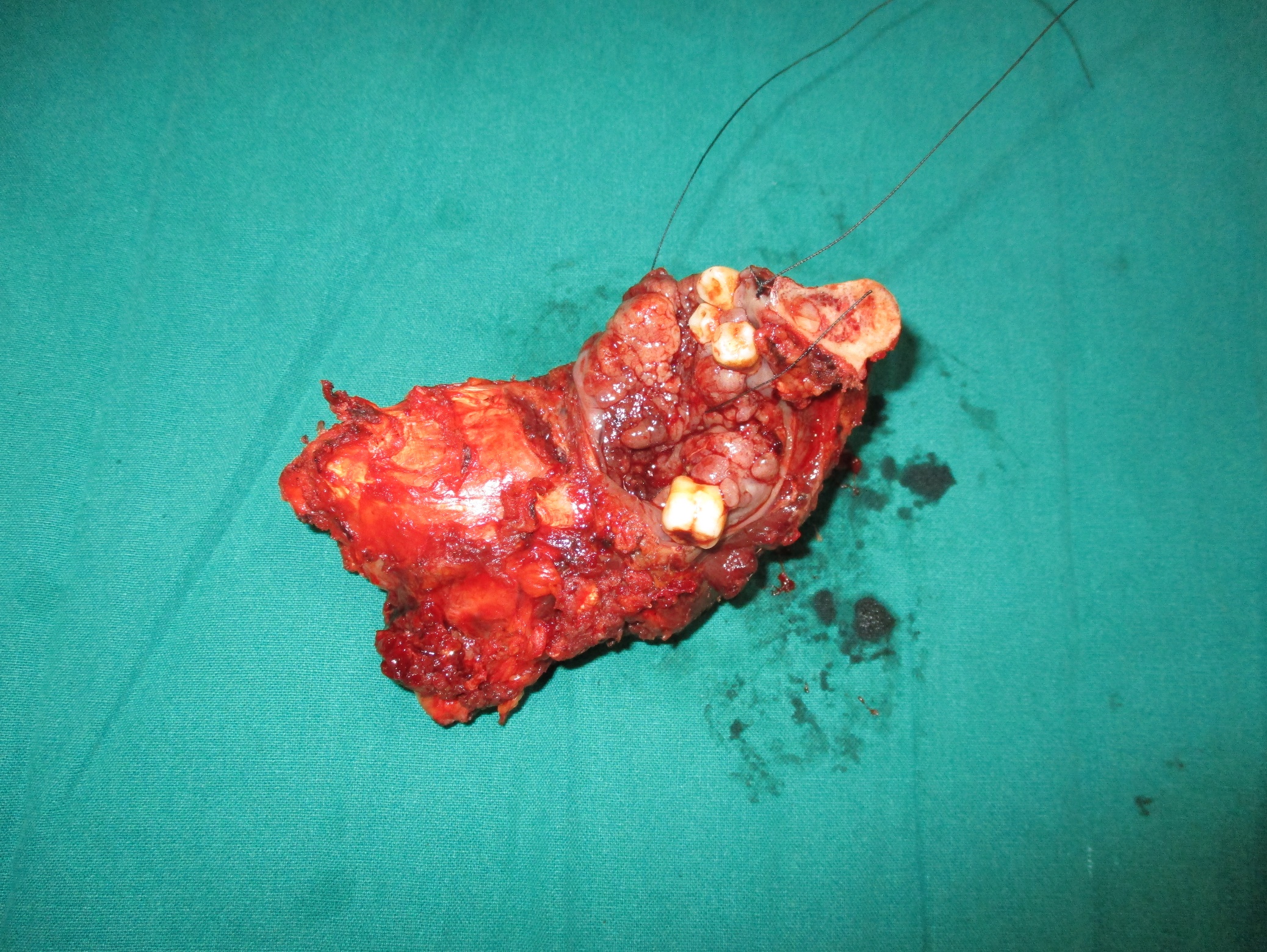
- Wide local excision of the involved part along with 1 to 2 cms of normal tissue
- Lymph Node dissection
- Reconstruction of the oral defect
Wide local excision
- The cancer tissue in the mouth is removed with a margin of 1 to 2 cms of normal tissue, depending on the part involved. A small margin of apparently normal tissue is removed along with cancer so that the microscopic seedlings of tumour tissue is also removed.
Lymph Node Dissection
- Oral Cancers spread to the lymph nodes in the neck. So, along with the tumour, the lymph nodes in the neck are also removed. This is called lymph node dissection. The lymph nodes removed are sent for biopsy to know whether they are involved in malignancy. This lymph node dissection helps remove the affected lymph nodes and allows us to decide on the subsequent treatment whether chemotherapy or radiotherapy is needed.
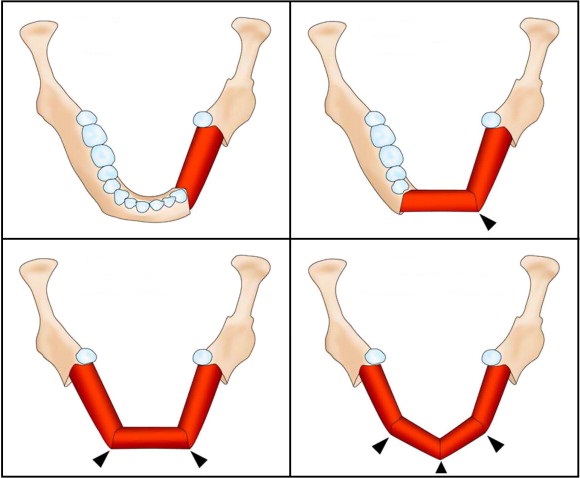
Reconstruction of the tumours
- After removing the tumour with a wide margin, there can be a significant defect that needs to be covered and reconstructed. Reconstruction helps to give form and symmetry to the face. The recent advances in technology have allowed us to use 3D printing technology to contour the new bone the same way as the native bone to attain facial symmetry giving a much superior cosmetic outcome.
What is the need for reconstruction after removal of oral cancer?
- Good reconstruction of the defects is essential to provide good outcomes in speech, eating, swallowing, and providing good symmetry to the face. Good reconstruction after oral cancer helps to improve the quality of life of the patient massively.
- After excision of the tumour, the tissues need to be closed and sutured back. The ability to reconstruct the defect after oral cancer surgery well gives the surgeon the confidence to excise the cancer with good margins. This will help improve the survival of the patient.
- Patients reconstructed well after oral cancer surgery look better than patients who have not been reconstructed.
- Thus reconstruction after oral cancer surgery becomes an integral part of cancer surgery and treatment.




How do we reconstruct after surgical removal of tumour?
Local flap reconstruction
- Local flap reconstruction involves replacing the defect with tissue from the adjacent area to cover the defect. Local flap reconstruction suits best when the defects are small, and there is sufficient tissue surrounding the area to cover and fill up the defect. If the defect is large and there is insufficient tissue to cover the defect, microvascular free flaps are more suitable.
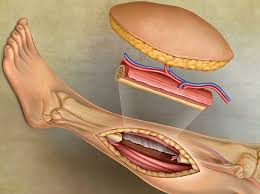
Microvascular free flap reconstruction.
- Microvascular free flap reconstruction remains the gold standard for reconstruction because it helps us provide adequate tissue for reconstruction, provide tissues such as bone, fat, and skin, improve the functional outcome, and maintain symmetry of the face. It also helps us to reduce the morbidity of the donor site.


Facts at a glance about surgery and post-operative instructions: ( May vary from person to person)
| Type of anaesthesia | General Anaesthesia |
|---|---|
| Surgery time | 2 - 6 hours |
| Hospital stay | 3 - 10 days |
| Mobilisation | 2nd day |
| Suture removal | 12th day |
| Self-care | 1-2 weeks |
| Full recovery | 4- 6 weeks |
| Return to work | 4 weeks |
What are the complications of surgery?
- Any procedure done can have complications. Although certain complications can happen in 5 to 10% of patients, every effort is undertaken to reduce surgical complications.
- Bleeding & Infection Although it is not common, bleeding and infection can occur in some individuals. If there is excess bleed, the patient might be taken back to the theatre, and the bleeding can be controlled. Wound infections usually settle with antibiotics and dressings.
- Flap loss In the head and neck, most patients are treated by free flap reconstruction. Here, the blood vessels in the flap are connected to the blood vessels in the neck to restore blood supply to the flap. However, in 2 to 3 % of patients, the connection between the blood vessels may not work, resulting in the loss of the flap. To prevent this, specialised nurses monitor the flap every hour for the first few days after surgery.
- Aspiration
What is expected in the post-operative period?
- Based on the extent of resection, the patient might be kept in a high dependency unit for a few days and then shifted to a room. Trained nurses will monitor the flap for the first few days.
- Feeding tube Since the significant part of the surgery involves the oral cavity, the patient might not be able to eat immediately due to pain. As the wounds need time to heal, a tube is passed through the nose into the stomach for feeding purpose thereby improving nutrition. The feeding tube will be removed once the patient can eat normally.
- TracheostomyIn case of large tumours and prolonged surgery, due to swelling in the airway, a hole is created in the neck through the windpipe few days ( approximately 5 -8 days). Once the airway swelling reduces, it is removed, and the patient can breathe normally.
What are the long term problems with oral cancer?
- Patients with advanced disease needing extensive surgery along with chemoradiotherapy might experience
- 1. Speech and Swallowing difficulties
- 2. Neck stiffness
- 3. Xerostomia
- 4. Trismus
- 5. Shoulder stiffness
- 6. Recurrence
- These problems can be minimised to a greater extent with careful surgical planning, good reconstructive surgical techniques, advanced radiotherapy, active physiotherapy and exercise in the post-operative period.
When will radiotherapy be necessary?
- Definitive Radiotherapy
When radiotherapy is used as the primary treatment method for oral cancers, it is called definitive radiotherapy. This is because radiotherapy can be used as an alternative to surgery to treat early cancers of the oral cavity in certain subsets such as commissure of lip and buccal mucosa. The results are almost equal to that of patients undergoing surgery.- Adjuvant Radiotherapy
When radiotherapy is given along with another form of treatment such as surgery to complement the treatment, it is called adjuvant radiotherapy. Adjuvant radiotherapy will be administered after surgery in case of advanced tumours or high-risk features like tumours greater than 4cms, depth greater than 10mm, involvement of the bone, neck node positivity, presence of lymphovascular invasion or perineural invasion.
When will chemotherapy be necessary?
- Definitive Chemoradiotherapy
When chemotherapy is used as the primary treatment method for oral cancers, it is called definitive chemoradiotherapy. Definitive radiotherapy is mainly used to treat inoperable tumours where surgery is not possible to attain negative margins.- Neoadjuvant Chemotherapy
When chemotherapy is given before surgery to downsize the size of the tumour, it is called neoadjuvant chemotherapy. This is occasionally done to preserve the mandible if it is close to the tumour.- Adjuvant Chemoradiotherapy
When chemoradiotherapy is given after surgery, it is called adjuvant chemotherapy. Adjuvant chemotherapy is given when high-risk features like positive margins for cancer and extranodal extension are present- Palliative Chemotherapy
Chemotherapy can be given in advanced cases and in metastatic cases where cancer has spread beyond the oral cavity to other organs prolong survival.
When will Targeted therapy be used?
- BasedTargeted therapy is a type of cancer treatment that uses drugs to precisely identify and attack specific types of genes and proteins involved in cancer growth. Targeted therapy will be used alone or in combination with chemotherapy in metastatic patients to prolong survival.
Can Oral Cancer come back? How can one identify the same?
- As in any cancer, there is always a chance that cancer can come back again. The possibility of oral cancer coming back depends on the stage of cancer, grade of cancer, the pattern of invasion, the positive margins involved and any adjuvant treatment received or not. So the patient will be kept under periodic follow up with clinical examination, CT/ MRI scan and endoscopy as required to identify recurrence. If the patient has any protruding growth or an ulcer not healing within 2 weeks or a neck swelling, the patient is asked to come back again for a checkup.
How will recurrence be treated?
- The diagnosis and treatment would be treated in the same way as primary cancers. An alternate treatment maybe used if the primary treatment modalities used can not be used in the patient.